Let’s face it: getting a referral for a specialist is no walk in the park. From the endless referral forms to dealing with insurance requirements and providers to choose from – booking an appointment can be a frustrating and long process.
You can easily get lost in this complex system, which, in turn, can prolong the waiting time even more, or you might end up paying more out of pocket.
That’s why understanding how doctor referrals work and how to navigate your insurance can make all the difference in your healthcare journey.
In this article, we’ll explore the ins and outs of doctor referrals and share how you can make the most of them to improve your health outcomes.
What Is a Doctor Referral and Why Do You Need One?
A doctor referral is essentially a recommendation from your primary care physician (PCP) to see a specialist who has more advanced expertise in a particular area of medicine—whether it’s a cardiologist for heart issues or a dermatologist for skin concerns.
Unlike a doctor’s order, which is a directive for specific tests or treatments (like lab work or X-rays), a primary care referral opens the door to specialized care by confirming that your condition requires a deeper level of expertise.
But why do you need a referral in the first place?
In many cases, it’s not as simple as picking up the phone and scheduling an appointment with any specialist. Health insurance companies have specific networks and protocols in place. An in-person or online doctor referral verifies that you truly need to see a specialist and that you’re staying within your insurance’s approved network. This keeps healthcare costs in check for both you and your insurance provider.
In many ways, referrals are about ensuring that you get the right care at the right time.
So, how do referrals work exactly?
How Do Doctor Referrals Work? A Step-by-Step Guide
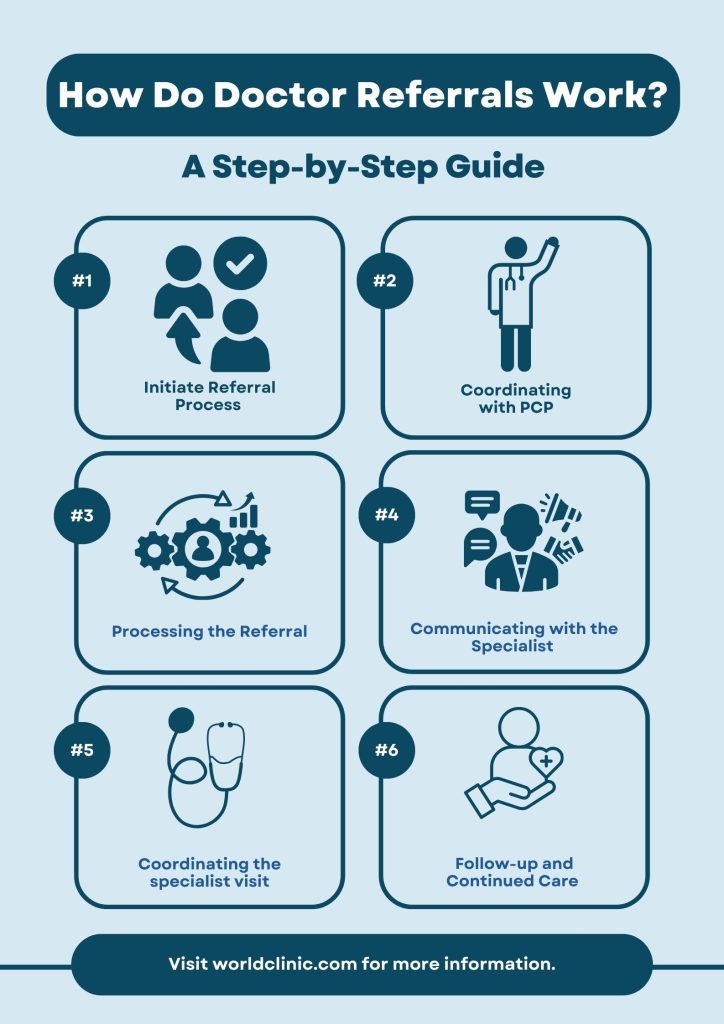
The medical referral process can be confusing, but once you know the steps, it becomes much easier to navigate.
Here are the 7 key steps of the referral process and what to expect along the way.
1. Initiating the Referral Process
If you’ve been dealing with symptoms that persist or worsen, first, you should contact your primary care physician.
Start by preparing a list of your symptoms, including how long they’ve been present and any patterns you’ve noticed. This helps your doctor get a full picture of your situation.
Schedule an appointment with your PCP, and during your visit, clearly communicate your concerns and why you think seeing a specialist could be beneficial. The more specific you can be, the easier it is for your doctor to determine the next best steps.
2. The PCP’s Role in Referrals
Once you request a referral, your PCP steps in as the central coordinator of your care. Their job is to assess your condition, possibly run a few preliminary tests, and determine if a specialist is needed.
If they agree that a referral is appropriate, they’ll choose a specialist who is also within your insurance network. Your PCP might also help determine whether the issue can be managed through primary care or if more advanced expertise is required.
Sometimes, a bit of patience is needed here—your PCP wants to make sure you’re being referred to the right specialist, which may involve gathering some additional information or doing initial tests.
3. Processing the Referral
Once your PCP decides on the referral, the paperwork begins.
But how long does a referral take to process?
Typically, it can take anywhere from a few days to a week for your referral to be processed.
This timeline can be affected by factors such as:
- Your insurance provider’s policies
- The availability of the specialist
- Your PCP’s office workflow
However, concierge medicine providers can speed up this process by providing more direct, personalized coordination between you, your PCP, and the specialist. Ultimately, concierge medicine accessibility ensures the referral process goes through without the usual delays or hurdles.
And if you’re wondering: how does concierge medicine work with insurance?
While the concierge medicine fee covers personalized care and services, you still need your insurance for specialist visits, hospital stays, and medications.
4. Communicating with the Specialist
Once the referral is approved, your PCP’s office will communicate directly with the specialist’s office. This is where your medical records, relevant test results, and any other background information are shared to ensure the specialist is filled in on your medical history.
The goal here is to make sure you don’t have to repeat tests or spend time explaining everything from scratch. The more coordinated this handoff, the more effective your specialist visit will be.
5. What to Expect During the Specialist Visit
When it’s time to see the specialist, it’s helpful to know what to expect. First, make sure you bring any referral documentation or specific records your PCP has provided. It’s also a good idea to prepare a list of questions or concerns you want to address during the visit.
Remember, this is your time to gain clarity about your health, so feel comfortable asking questions and discussing treatment options.
6. Follow-up and Continued Care
After your visit, it’s important to follow up with your PCP. Often, the specialist will send a report back to your PCP outlining their findings and treatment recommendations.
This ensures continuity of care, as your PCP will stay in the loop about your condition and any further treatments or referrals that may be needed. Keep an open dialogue with both your PCP and specialist to make sure everyone is aligned on your care plan.
Navigating Insurance and Referrals
Knowing what your insurance covers, which specialists are in-network, and whether pre-authorization is required can make a big difference in both your out-of-pocket costs and the timeliness of your care.
Understanding Insurance Types and Referrals
Health insurance plans come in various types, and each has its own rules when it comes to referrals.
- HMOs (Health Maintenance Organizations) generally require that you get a referral from your primary care physician before seeing any specialist. This ensures that care stays within their network and helps control costs.
- PPOs (Preferred Provider Organizations) offer more flexibility—you don’t always need a referral, and you can see out-of-network providers, though you’ll pay more for that freedom.
- POS (Point of Service) plans combine elements of both HMOs and PPOs, requiring referrals for specialists while still allowing some out-of-network care at higher costs.
Pre-Authorizations and Insurance Approvals
In many cases, before you can even schedule an appointment with a specialist, your insurance company may require a pre-authorization. This means that your insurer needs to approve the referral, and the specialist visit to ensure its medical necessity.
It’s essentially the insurance company’s way of managing costs and making sure you’re receiving appropriate care. If pre-authorization is required but not obtained, your visit might not be covered, leaving you with the full bill. To avoid this scenario, check with your PCP or insurance provider ahead of time to avoid delays or surprise expenses.
In-Network vs. Out-of-Network Referrals
When it comes to insurance, staying in-network is key to keeping costs manageable.
In-network providers have agreed-upon rates with your insurance company, which means lower costs for you. If you go out-of-network, the charges can skyrocket, and in some cases, your insurance may not cover the visit at all.
This is why you should confirm that the specialist your PCP refers you to is within your network.
Common Issues with Referrals and How to Avoid Them
The referral process can be filled with complications—whether it’s waiting for insurance approval, misunderstanding coverage, or struggling to access the right specialists.
That’s where concierge medical services like WorldClinic make a difference. By handling the complexities of the referral process, from ensuring timely approvals to finding the right specialists, WorldClinic ensures that members receive seamless, stress-free care.
WorldClinic offers a tailored approach to healthcare coordination to meet your specific needs, including:
- While traveling: Travelers often face the challenge of accessing trusted healthcare providers in unfamiliar locations. WorldClinic’s Silver membership is designed for frequent travelers, providing expedited worldwide doctor referrals. This helps with travel risk management, ensuring you have reliable medical support wherever your travels take you.
- While home or away: For those who value convenience and around-the-clock healthcare access, WorldClinic’s Gold membership is the ideal solution. This tier adds the benefit of sourcing and vetting top local primary care physicians, ensuring that members always have access to the best care, no matter where they are or what time it is.
- For every aspect of care needs: For busy professionals and executives, managing healthcare alongside a demanding schedule can feel overwhelming. WorldClinic’s Platinum membership offers comprehensive healthcare management, from coordinating annual executive physicals to handling appointment scheduling and ongoing care management.
Conclusion: Taking the Confusion Out of Doctor Referrals
Dealing with doctor referrals doesn’t have to be stressful. By understanding how the process works and choosing a healthcare service that handles the details for you, you can save time and avoid unnecessary delays.
By offering tailored care coordination services, WorldClinic ensures that referral challenges become a thing of the past. With customized membership plans that cater to your unique lifestyle, WorldClinic takes the guesswork out of healthcare, making it easier for you to focus on what matters most—your health.
Doctor Referrals: FAQs
How Can I Check If My Insurance Requires a Doctor Referral?
The best way to check is by reviewing your insurance plan details, either through your insurer’s website or by calling their customer service. Your primary care physician can also help clarify whether a referral is necessary for your situation.
How Does a Doctor Referral Impact My Healthcare Costs?
Referrals help ensure that your visit to a specialist is covered under your insurance, which typically lowers your out-of-pocket costs. Without a referral, you may be billed at a higher rate, or the visit might not be covered at all
How Are Doctor Referrals Handled in Emergency Situations?
In emergencies, referrals are generally not required. Emergency room doctors will provide immediate care and, if necessary, connect you to specialists without waiting for the formal referral process.
How Can Concierge Care Speed Up the Medical Doctor Referral Process?
Concierge care services like WorldClinic offer direct coordination between your doctor and specialists, eliminating long wait times for referrals and ensuring quicker access to the care you need.
Can I See a Specialist Without a Referral in Concierge Medicine?
Yes, in many cases, concierge medicine allows you to bypass the traditional referral process, offering more immediate access to specialists as part of the service.
Can Urgent Care Give Referrals to Specialists?
Yes, urgent care providers can give referrals if they determine that you need specialized care after evaluating your condition. However, you may still need to confirm this referral with your insurance provider. For more insights into the roles of each, see our guide on urgent care vs primary care to understand which service best suits different healthcare needs.


