Care continuity helps patients receive the right care at the right time from their healthcare providers. This concept aligns with modern healthcare’s patient-centered models, where treatments prioritize individual needs and value-based frameworks.
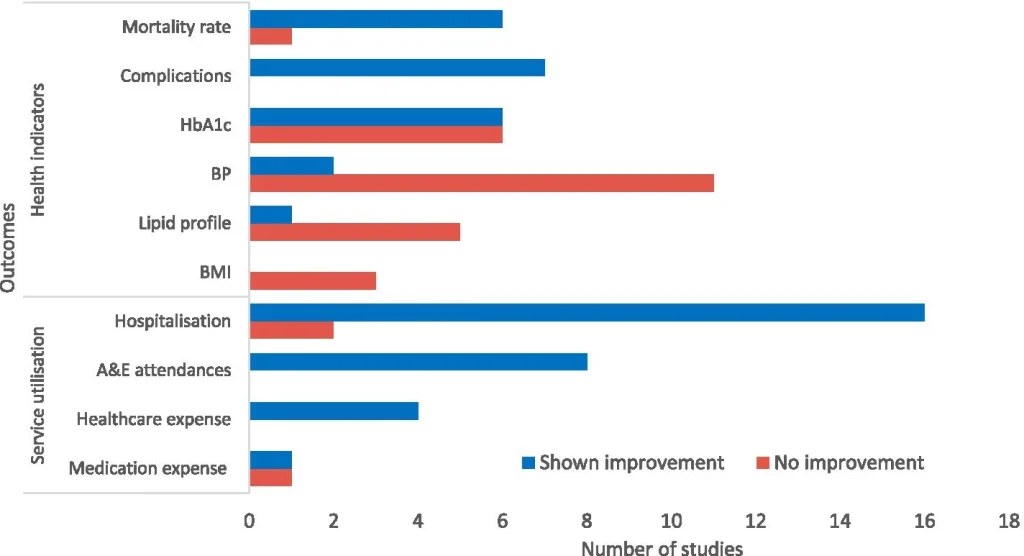
Research shows that strong care continuity reduces mortality rates in 81.8% of cases. Patients who maintain regular contact with their primary care physician experience fewer hospital admissions, reduced healthcare costs, and higher satisfaction levels. These patients also develop stronger trust relationships with their healthcare providers.
For healthcare systems, focusing on care continuity leads to better patient health, fewer return hospital visits, and more effective use of medical resources.
In this guide we will explain what continuity of care means, how it fills gaps in treatment, and what steps healthcare providers can take to improve patient care.
What is Care Continuity?
The definition of continuity of care centers on maintaining an ongoing, trusted relationship between patients and providers across multiple interactions. Healthcare teams work together to give patients the care they need as their health changes – this includes regular checkups, visits to specialists, and care after leaving the hospital. To make this work, healthcare providers must:
- Share complete patient health records with each other
- Consistent communication between each other about patient care
- Check on patients regularly after treatments
Among many examples of continuity of care, consider how a primary care physician collaborates with a cardiologist to manage a patient’s hypertension. Both doctors know the patient’s full medical history, medications, and treatment plan. This teamwork ensures the patient receives consistent, effective care at every visit.
Why Continuity of Care Is Important?
Healthcare organizations that focus on continuity of care achieve better results for their patients while reducing costs across their systems. These improvements stem from several connected benefits that strengthen overall patient care.
Improved Health Outcomes
When patients see the same healthcare team regularly, their doctors build a deep understanding of their health patterns and needs. This knowledge enables medical teams to catch potential problems early through consistent monitoring and timely interventions. As a result, patients manage their ongoing health conditions more effectively, leading to better outcomes.
Above mentioned research strongly supports this approach: 81.8% of studies show that patients who receive continuous care live longer than those who don’t.
Patients with ongoing health conditions also need fewer hospital stays when they get care and continuity from their primary doctor.
Enhanced Patient Satisfaction
Strong relationships between patients and their regular healthcare providers create a foundation for better care experiences. Since these providers already know each patient’s medical history, appointments focus on current health needs rather than reviewing past information. This efficiency not only saves time but also builds patient trust.
Studies confirm this connection between continuity in care and patient satisfaction. When patients trust their medical team, they become more likely to follow their treatment plans and participate actively in their care.
Avoided Treatment Gaps
Healthcare teams use care continuity to create a safety net that catches potential gaps in treatment. They actively track appointments and treatments while maintaining communication between all healthcare providers involved in a patient’s care. Clear communication protocols ensure patients attend critical follow-up appointments and receive care at the right time.
This coordinated approach ensures smooth transitions between different types of care, from regular check-ups to specialist visits. By connecting all aspects of care and continuity, medical teams prevent treatment gaps and address health issues before they become serious problems.
Significant Cost Savings
Studies show that improved health outcomes from care continuity directly reduce medical expenses for both patients and healthcare systems. Because patients receive regular preventive health care, they require fewer emergency room visits and hospital stays.
This reduction in urgent care needs allows healthcare organizations to shift resources from expensive emergency treatments to more cost-effective preventive care programs. The savings then support further improvements in patient care services.
Strategies to Enhance Care Continuity
We will now explore practical steps healthcare organizations can take to improve continuity in care. These strategies work together to create a more connected healthcare experience for every patient.
1. Develop Interdisciplinary Care Teams
Care continuity works best when different healthcare professionals collaborate on patient treatment. Primary care doctors work closely with nurses, specialists, pharmacists, and therapists to understand each patient’s full health picture.
Each of them brings specific medical knowledge that helps create complete treatment plans. For example, a pharmacist might notice a potential drug interaction that affects a patient’s physical therapy plan. By sharing information this way, patients receive safer, more effective care.
2. Streamline Electronic Health Records (EHRs)
Strong continuity in care leverages the benefits of electronic health records. When all healthcare providers use the same EHR system, they have quick access to patient information including:
- Past medical treatments
- Current medications
- Test results
- Treatment plans
When healthcare teams use EHRs correctly, they avoid repeating tests or giving conflicting treatments. This saves time and money while keeping patients safer.
3. Standardize Communication Protocols
Clear communication rules help healthcare teams work together smoothly. Organizations should create standard forms for sharing patient information between departments and providers. These rules should include:
- Detailed checklists for transferring patient care between providers
- Secure messaging systems that follow HIPAA privacy rules
- Leveraging the benefits of telemedicine for patient appointments and team meetings
These checklists help maintain continuity in care by keeping all healthcare providers informed about their patients’ needs.
4. Leverage Executive Health Partnerships
Working with executive health programs like WorldClinic shows show how care and continuity work best. They offer services that every healthcare organization can learn from:
- Medical teams available 24 hours a day
- Immediate appointment scheduling
- Comprehensive yearly health assessments
Healthcare organizations can use these high-touch examples of continuity of care to improve services for all patients. This creates better connections between patients and their healthcare teams while making care easier to access.
The Challenges of Care Continuity
Achieving seamless care continuity requires overcoming barriers that affect patients, families, and providers alike. Below are common challenges and strategies to address them:
1. Disconnected Care Teams
When several healthcare providers work separately, care continuity can become disorganized. Centralized coordination—such as WorldClinic’s care coordination model—assigns a central point of contact to synchronize updates across specialists. A main contact person helps by:
- Keeping track of all medical treatments
- Making sure all providers know about changes in care
- Setting up appointments with different doctors
- Creating one clear treatment plan for everyone to follow
This approach works well for individual patients, families, and large organizations alike.
2. Lack of 24/7 Availability
Patients need medical help at all hours, not just during office visits. A concierge model ensures real-time support via telehealth or direct provider access, through which healthcare organizations can provide:
- Round-the-clock access to medical advice
- Quick responses to urgent health questions
- Easy ways to schedule urgent appointments
- Clear guidance for after-hours care
This accessible care continuity model works well for individuals, families, and employers who need healthcare support at any time.
3. Incomplete Patient Records
Missing or scattered medical information makes it hard to provide good care continuity. Healthcare teams need:
- One complete record system
- Quick access to patient information
- Regular updates to patient records
- Clear documentation standards
Unified, interoperable EHR systems consolidate records, enabling accurate diagnoses and timely interventions for all patients.
4. Compliance and Security Concerns
Sharing patient information safely requires strict security measures. Healthcare organizations must:
- Follow HIPAA privacy rules
- Protect patient data during transfers
- Secure all communication channels
- Train staff on data protection
These needs should be addressed with secure electronic health records and strict privacy protocols that protect patient information while maintaining care continuity.
5. Minimal Personalized Follow-Up
Standard after-care instructions often miss important details that different patients need. Everyone has unique health needs – busy professionals need flexible scheduling, families with children need age-appropriate care plans, and people with ongoing health conditions need regular monitoring. Personalized medical care strategies should include:
- Check-ins that fit each person’s schedule
- Care instructions that match daily routines
- Regular updates based on changing health needs
- Support that works with different lifestyles
WorldClinic demonstrates how customized follow-up care helps different types of patients stay on track with their health goals. Their approach shows how personal attention makes a difference in care continuity, whether for a working parent, a child with special needs, or someone managing a long-term condition.
6. Administrative Overload
Complex paperwork and insurance checks often delay healthcare for everyone, from company employees to individual patients. A streamlined approach, like a concierge care model, helps by:
- Making appointment scheduling quick and simple
- Speeding up insurance verification
- Simplifying the process of seeing specialists
- Reducing paperwork between different healthcare providers
- Shortening wait times for appointments and treatments
This efficient care model shows how removing administrative barriers helps all patients get care faster. This approach works well for both large employer health programs and individuals who want more personal attention. When healthcare teams spend less time on paperwork, they can focus more on patient care.
Conclusion
Care continuity makes healthcare work better for everyone. When healthcare teams stay connected, share information, and track patient care actively, they help patients stay healthier and spend less on medical care.
Effective care continuity depends on:
- Healthcare teams working together
- Complete, accessible patient records
- Clear communication between providers
- Regular patient follow-up
- Easy access to medical care
WorldClinic’s on-demand concierge medical services shows how modern care continuity works in practice. Their approach combines 24/7 medical support, coordinated care teams, and personal attention to patient needs. This model helps prevent gaps in treatment, increases patient satisfaction, and makes healthcare easier to access.
Ready to experience better healthcare? WorldClinic offers membership plans that fit different needs:
- For individuals and families
- For employers and organizations
- For healthcare providers
FAQs About Care Continuity
1. What is continuity of care, and why is it so crucial for patient outcomes?
Continuity of care is the ongoing relationship between patients and their healthcare providers that ensures consistent, coordinated medical care over time. This care approach improves patient survival rates, reduces emergency visits, enhances treatment adherence, and leads to better overall health outcomes.
2. How do tools like telehealth and remote monitoring enhance continuity of care?
Telehealth and remote monitoring strengthen continuity in care by breaking down access barriers and enabling constant connection between patients and providers. These digital tools allow healthcare teams to monitor patient health in real-time, conduct virtual follow-ups, and quickly address concerns before they become serious issues.
3. How can healthcare organizations measure the effectiveness of their continuity initiatives?
Healthcare organizations can evaluate care continuity effectiveness through several key metrics:
patient satisfaction rates
reduction in hospital readmissions
emergency department visit frequencies
overall health outcomes
Studies show that higher continuity of care correlates with fewer hospital admissions for conditions that could be managed through regular outpatient care.
4. How does an on-demand or concierge model fit into the broader conversation around care continuity?
The on-demand and concierge medicine model exemplifies modern care continuity by providing 24/7 access to healthcare providers, coordinated care teams, and personalized attention. This approach offers several benefits: it ensures that patients can always reach their healthcare team, receive prompt care coordination, and maintain consistent relationships with their providers.
5. Can improved care and continuity help reduce overall healthcare costs in the long run?
Yes, strong care continuity leads to cost savings. Studies demonstrate that patients with consistent primary care relationships experience fewer emergency department visits and hospitalizations, resulting in lower healthcare costs. Regular preventive care and early intervention through continuous care relationships help avoid expensive emergency treatments and reduce the need for costly hospital stays, creating long-term savings for both patients and healthcare systems.


