The global pandemic dramatically accelerated healthcare transformation, pushing providers and patients to embrace remote solutions at unprecedented rates. Virtual care became an essential service, connecting patients with needed healthcare through telemedicine, remote monitoring, and digital health platforms.
Research has demonstrated that virtual care provides safe and appropriate options for initial assessment and delivers comparable results to traditional visits, particularly for counseling and rehabilitation services. It provides convenience with maintained clinical quality, giving patients effective care options regardless of their location.
This comprehensive guide explores what virtual care is, examines its types, highlights its benefits, and discusses how healthcare systems can implement it more widely.
What is Virtual Care?
Virtual care includes all methods healthcare providers use to interact with patients remotely. It refers to any clinical interaction that doesn’t involve direct physical contact between provider and patient, instead using technology to deliver care.
Currently, 78% of hospitals have already implemented a virtual care solution and removed geographical barriers to evaluate, diagnose, and treat patients through secure digital channels.
Virtual healthcare includes video consultations, telephone appointments, secure messaging, remote monitoring, and digital health applications. These technologies create comprehensive remote care options that extend beyond traditional facility limitations.
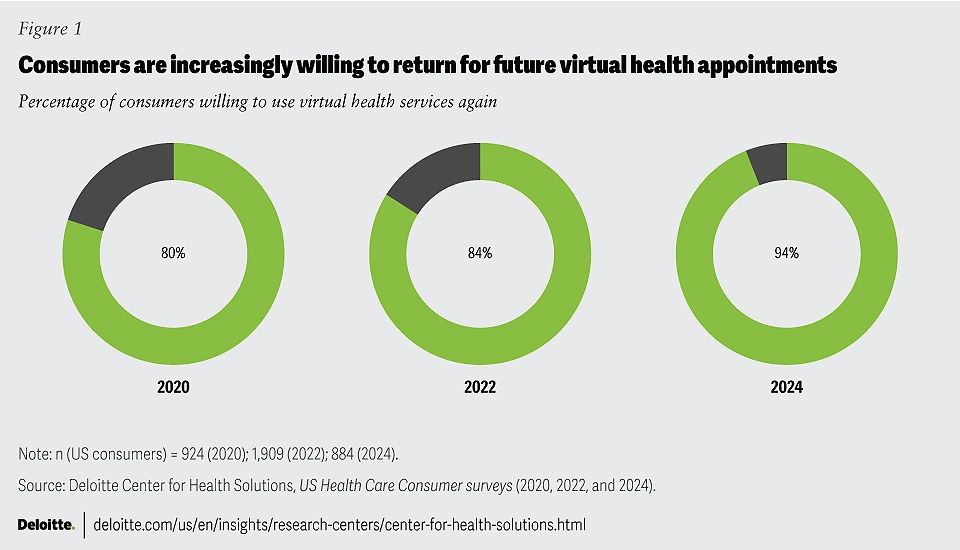
Notably, about 24% of surveyed patients indicate they would switch doctors to ensure access to virtual health options. This growing preference signals a fundamental shift in patient expectations, with more individuals actively seeking providers who offer flexible, technology-enabled care options.
Key Components of Virtual Care
Virtual care is built on several core components that work together to deliver comprehensive remote healthcare services. Below, we break down these components and explain how they contribute to efficient healthcare delivery.
Telehealth
The primary and the most well-known component of virtual care is telehealth, which focuses on real-time remote consultations between patients and healthcare providers. These consultations occur through video conferencing, telephone calls, or secure messaging platforms.
This method is widely used for routine check-ups, mental health therapy, and specialist consultations. The benefits of telemedicine are not only increased accessibility for patients living in remote or underserved areas but also reduced travel time and associated costs.
Remote Patient Monitoring (RPM)
Another component of virtual care is Remote Patient Monitoring (RPM), which uses connected devices and wearable technology to track health metrics and send this information to healthcare providers.
RPM is particularly valuable in chronic disease management and preventive health approaches. This virtual care type helps providers detect concerning signs early and prevent complications. It is frequently used for patients with chronic conditions.
Digital Health Solutions
Virtual care also includes various digital health solutions like mobile apps, AI-powered chatbots, and online health portals. All these technologies help patients and providers to track symptoms, schedule appointments, and access medical records.
When integrated with electronic health records (EHR), they enhance care coordination, improve patient experience, lower costs, and enhance clinician experience (JMIR).
Virtual Care vs. Telehealth: Understanding the Distinctions
While telehealth is an important component of virtual care, they are often used interchangeably and cause confusion. So, let’s clarify these important concepts:
- Virtual care functions as the broader category including all technology-enabled remote healthcare services. It includes any clinical interaction where provider and patient aren’t physically together.
- Telehealth or telemedicine specifically refers to the technology and methods enabling remote clinical services through telecommunications.
Below is a comparison table for a more detailed review of the key differences between virtual care and telehealth:
| Aspect | Virtual Care | Telehealth |
|---|---|---|
| Scope | It includes all remote healthcare services, including RPM, digital tools, and telehealth. | Primarily focuses on real-time remote consultations. |
| Components | Includes telehealth, remote patient monitoring, and digital health solutions. | One component within the larger virtual care ecosystem. |
| Data Integration | Often integrates with EHR systems and other digital health records for comprehensive care. | Typically focuses on direct patient-provider interaction. |
| Usage | Broad applications ranging from preventive health to chronic disease management. | Mainly used for routine consultations and follow-up visits. |
Understanding these distinctions between virtual care vs telehealth helps clarify the broader benefits of virtual healthcare and supports informed decision-making for both patients and providers.
5 Benefits of Virtual Care
The advantages of virtual care extend beyond the convenience of remote consultations. Several benefits have been identified through research and practice, improving how patients receive services and how providers deliver them.
1. Enhanced Accessibility and Convenience
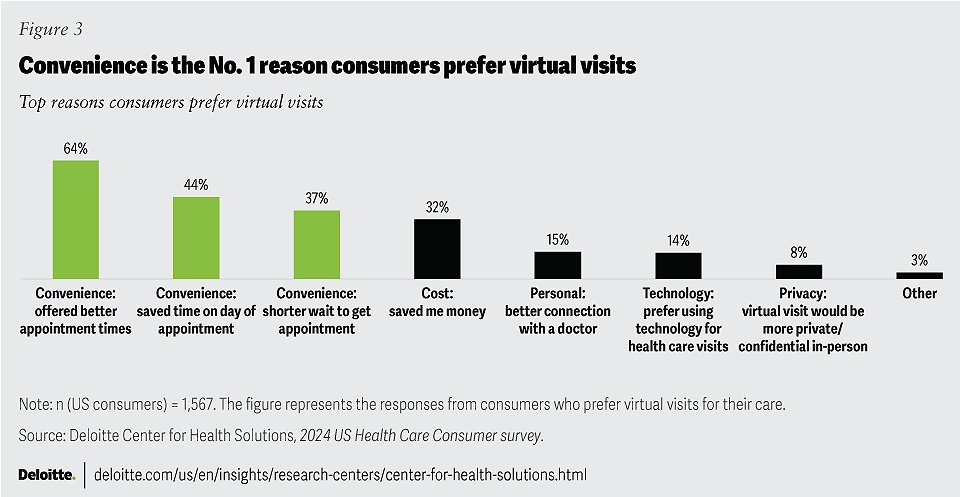
One of the first benefits of virtual care is improved access for patients in rural areas, those with mobility limitations, and individuals with demanding schedules. Patients can connect with providers from home, work, or while traveling, eliminating transportation challenges and reducing time away from responsibilities.
This convenience leads to higher appointment completion rates. Research shows telemedicine appointments are more likely to be completed than traditional visits, addressing the persistent challenge of appointment no-shows that disrupt care delivery and practice efficiency.
2. Lower Healthcare Costs
Virtual care reduces healthcare costs through multiple mechanisms. Patients save on transportation expenses, parking fees, and lost wages from missed work. Healthcare systems benefit from more efficient resource use, reduced overhead for physical facilities, and fewer unnecessary emergency department visits.
3. Improved Clinical Outcomes
Remote patient monitoring, a crucial component of virtual care, has demonstrated significant clinical benefits, including a 50% reduction in hospital readmissions for patients with heart conditions. This improvement occurs because continuous monitoring allows early intervention before complications require emergency care.
Through RPMs, virtual care also maintains care continuity by keeping patients connected with their healthcare teams. This consistent engagement leads to better adherence to treatment plans and more effective management of chronic conditions.
Studies also indicate that virtual consultations are equally or more effective than face-to-face care for managing certain conditions, particularly mental health concerns.
4. Reduced Wait Times & Faster Care
Virtual care reduces wait times typically associated with in-person visits. Patients receive medical advice, prescriptions, and follow-up care without waiting for physical clinic appointments. For non-emergency conditions, this quick access to medical guidance prevents potential complications and supports preventive health.
5. Better Chronic Disease Management
Virtual care improves the management of chronic conditions through continuous monitoring and personalized medical care. Patients with diabetes, hypertension, or heart disease can check in with providers regularly, track their health data, and receive treatment adjustments without frequent office visits.
How Virtual Care Transforms Healthcare Delivery
Virtual care improves healthcare delivery at every point of care. Here’s how it benefits patients, employers, and health systems.
For Individuals & Families
For patients and their support networks, virtual care eliminates common barriers to healthcare access. Virtual care has made membership medicine more accessible to deliver, expanding access to personalized healthcare services through various models. The concierge model represents one of these approaches, offering premium services with direct provider access.
Concierge family medicine is a prime example of this integration, providing families with comprehensive care management and 24/7 medical support through virtual platforms. Families can monitor the health conditions of all members, from children to elderly parents, without disrupting their daily schedules. This accessibility results in more consistent care and earlier intervention.
For Employers
Virtual care for employers creates substantial workforce and operational benefits. These programs enhance employee wellness initiatives by providing immediate access to healthcare providers, and reducing time away from work for routine medical appointments. Companies report decreased healthcare costs as employees address health concerns early, preventing more expensive treatments later.
Organizations implement virtual care in various ways based on their specific needs. Some companies focus on travel risk management to support employees during business trips, while others leverage the benefits of concierge medicine for executive-level healthcare support. This flexibility allows businesses to tailor virtual care solutions to their workforce requirements.
For Health Systems
Health systems using virtual care experience streamlined operations through optimized provider scheduling, reduced no-show rates, and more efficient utilization management. These improvements allow for better resource allocation and capacity management. The data generated through digital interactions enables more sophisticated population health management and predictive analytics capabilities.
Challenges and Considerations in Virtual Care Implementation
While virtual care offers significant benefits, successful implementation requires addressing several important challenges.
1. Technological Barriers
Effective virtual care requires reliable technical infrastructure including high-speed internet, compatible devices, and secure platforms. Both providers and patients need appropriate technology access and sufficient digital literacy to participate fully.
2. Regulatory Requirements
Healthcare providers who implement virtual care face specific regulatory challenges. These include state-by-state licensing rules, provider credentialing, and insurance policies that vary by location. Organizations may need dedicated staff to track and respond to regulatory updates
3. Data Security and Privacy
Virtual care requires strict protection of patient health information during virtual visits, data transmission, and storage. Healthcare providers must use secure platforms that comply with privacy regulations. This includes encrypted video connections, protected health record access, and secure messaging systems between providers and patients.
5. Quality of Care
Maintaining high standards of care in a virtual setting presents unique challenges. Providers need specific protocols for conducting thorough virtual examinations and clear criteria for determining when in-person visits are necessary. Building trust between patients and providers requires consistent communication and reliable virtual care experiences.
Integrating Virtual Care with Comprehensive Health Support
The most effective virtual healthcare models go beyond basic telehealth consultations, creating integrated systems that provide continuous, proactive, and coordinated care regardless of patient location.
24/7 Immediate Physician Access
Advanced virtual care platforms provide round-the-clock access to experienced physicians familiar with patients’ medical histories, leveraging the benefits of electronic health records. This continuous availability ensures personalized treatment and rapid response to health concerns whether patients are at home or traveling.
Unlike episodic urgent care interactions, these personalized medical care relationships deliver contextualized guidance from providers who understand patients’ complete health profiles. This approach combines the convenience of on-demand care with the quality benefits of consistent provider relationships, supporting both acute needs and ongoing health management.
Personalized Medical Preparedness
Comprehensive virtual care programs provide patients with personalized prescription kits and diagnostic tools, enabling better health risk assessment and management of common illnesses, minor injuries, and chronic condition fluctuations. Having physician-selected medications and guidance readily available improves response times and builds patient self-efficacy.
Global Reach with Local Expertise
Sophisticated virtual care platforms provide consistent, high-quality medical oversight across different states and countries. Through care coordination networks, patients receive expert guidance navigating unfamiliar healthcare systems when traveling while maintaining a connection with their primary care team.
This global-local approach ensures continuous support regardless of location, combining the benefits of an integrated health system with the flexibility modern patients require. For organizations with mobile workforces or individuals who travel frequently, this capability changes healthcare from a location-dependent service to a continuous resource.
Conclusion
Virtual care represents more than a temporary pandemic adaptation—it marks a fundamental change in healthcare delivery. By combining telehealth consultations, remote monitoring, digital health tools, and coordinated support systems, virtual care creates more accessible, efficient, and patient-centered healthcare experiences.
The evidence demonstrates that virtual approaches maintain or improve clinical outcomes while enhancing convenience and reducing costs. As technology advances and regulatory frameworks mature, virtual care will further integrate into mainstream healthcare delivery, becoming an expected component of comprehensive medical services.
Discover Our Membership Plans
Take advantage of modern virtual care solutions that work for you. WorlClinic’s concierge medical services combine virtual care with personalized support for better results.
Through our membership plans, you receive coordinated care that fits your specific healthcare needs.
Get high-quality care that’s always available, no matter where you are
Experience Personalized Healthcare Anywhere, Anytime
Discover how WorldClinic’s Concierge Telemedicine Services put world-class medical expertise at your fingertips. From 24/7 access to tailored medical solutions, our memberships ensure peace of mind and proactive care for you and your family.
.
FAQ About Virtual Care
1. Can virtual care replace in-person doctor visits?
Virtual care serves as an effective complement to in-person care rather than a complete replacement. While many conditions can be diagnosed and treated remotely, certain medical situations require physical examinations, procedures, or tests that must be performed in person. Healthcare providers assess each case to determine the most appropriate care delivery method based on the patient’s specific needs and medical condition.
2. How does remote patient monitoring work in virtual care?
Remote Patient Monitoring uses connected medical devices to track patient health data and send it directly to healthcare providers. Patients use prescribed devices at home to measure vital signs such as blood pressure, heart rate, blood glucose, or oxygen levels. These devices automatically transmit readings to secure medical platforms where providers analyze the data and adjust treatment plans as needed.
3. Is virtual care effective for managing chronic conditions?
Studies demonstrate that virtual care effectively manages chronic conditions through consistent monitoring and timely interventions. Virtual care allows providers to track symptoms, adjust medications, and address complications early. This approach works particularly well for conditions like diabetes, hypertension, and heart disease that require regular monitoring.
4. How can employers integrate virtual care into employee health programs?
Employers can integrate virtual care into their health programs through several practical steps.
First, select a virtual care platform that meets employee healthcare needs and integrate it with existing health benefits.
Next, create clear policies about virtual care usage and coverage.
Then, provide employee training on accessing and using virtual care services.
5. Does insurance cover virtual care services?
Insurance coverage for virtual care varies by provider, plan type, and location. Many insurance companies now cover video consultations, remote monitoring, and other virtual services similarly to in-person visits, particularly since the pandemic.
However, coverage policies continue to evolve. Patients should verify specific virtual care benefits with their insurance providers, including any applicable copays, deductibles, or coverage limitations.


