Have you ever wondered if genetic testing might benefit your health journey? Let’s talk about this increasingly popular medical option. Genetic testing offers insights into your risk for certain health conditions, but it also raises some important ethical and practical concerns.
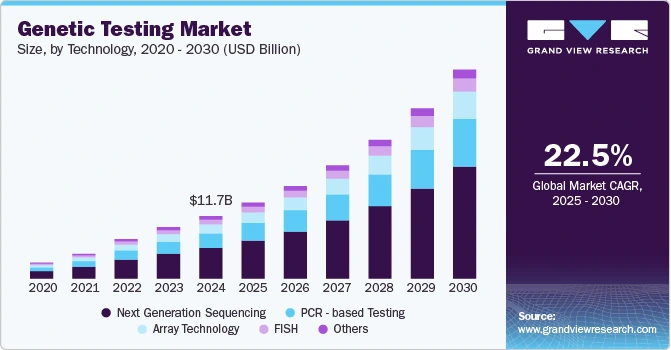
A recent survey showed that about 81% of Americans are aware of genetic testing, and its usage has increased from 19% in 2020 to roughly 40% in 2022. Even with this growing interest, deciding to get tested is a personal choice – and many people are unsure if it’s the right move.
In this article, we’ll explore both the pros and cons of genetic testing to help you make an informed decision. You’ll learn what genetic testing involves, the different types available, and how it can influence your health choices.
We’ll also discuss major challenges surrounding genetic information and how a supportive healthcare approach – like concierge medicine – can guide you through the process. By the end, you should have a balanced understanding to make the choice that’s best for your health.
What Is Genetic Testing?
Let’s start with the basics. Genetic testing analyzes your DNA to identify mutations, inherited traits, or genetic markers linked to various diseases. It’s essentially a way to peek at your genetic instruction manual.
These tests help assess your health risks, medication responses, and inherited conditions by examining changes in your chromosomes, genes, or proteins. You can think of it as a specialized health risk assessment focused specifically on your genetic makeup.
The science behind it is pretty straightforward: your DNA contains instructions for cell development and function and changes in these instructions can affect your health.
You can get genetic testing through blood, saliva, or tissue samples. Each method works best for different kinds of tests. The lab will examine specific sections of your DNA or your entire genome to find variations that might impact your health.
For example, discovering a high-risk cancer gene might lead doctors to start screenings earlier, and finding a variant affecting how a patient processes a medication could prompt the choice of a different drug or dose that’s better for them.
Genetic testing is becoming routine in medicine – over 90% of genetic tests in the U.S. are done for clinical purposes, and about 62.1% are for diagnostics. In short, genetic testing helps in personalized medical care by giving you and your doctors information unique to your DNA.
7 Types of Genetic Testing
Let’s discuss the different types of genetic tests available, each serving a specific purpose. Depending on your situation, you might encounter one or more of the following:
1. Full Body Tests
Advanced medical technologies now offer comprehensive physical and genetic assessments. These include whole-body imaging like MRIs and CT scans, alongside extensive genetic analyses such as Whole Genome Sequencing (WGS) and Whole Exome Sequencing (WES).
While these tests provide unprecedented insights into your health, they share common challenges. Both imaging and extensive genetic tests frequently identify “incidental findings” – anomalies that appear concerning but are often benign. These discoveries can trigger unnecessary anxiety and lead to a cascade of additional tests, some carrying their own risks.
More concerning is when patients receive these detailed results but experience a complete lack of follow-up care. The solution lies in a personalized approach to testing. Rather than undergoing universal screenings, patients benefit most from tests tailored to their specific health profile and risk factors. When comprehensive tests are performed, proper care coordination ensures thorough follow-up, including appropriate specialist referrals and monitoring plans.
2. Predictive & Presymptomatic Testing
These tests spot genetic mutations that might increase your disease risk before symptoms appear. For example, checking for BRCA gene mutations in someone with a family history of breast or ovarian cancer.
Why consider this type of testing? It can motivate you to take preventive measures and get enhanced screening, potentially catching conditions when they’re more treatable. If you have a family history of hereditary conditions, these tests could help you make informed health decisions.
3. Carrier Testing
Are you worried about passing genetic conditions to your children? Carrier testing determines if you carry gene mutations that could cause inherited disorders like cystic fibrosis or sickle cell anemia in your children.
It’s often used by couples planning a baby to understand reproductive risks and explore options. It’s especially relevant if you come from ethnic backgrounds with higher frequencies of certain genetic disorders or have known family histories of recessive conditions.
4. Diagnostic Testing
When symptoms already exist, diagnostic testing confirms or rules out suspected genetic conditions. About 5%–10% of all cancers come from harmful genetic changes inherited from a parent.
These tests can end the lengthy search for answers that many patients with rare diseases experience. They provide clarity and direction for medical management by analyzing specific genes or broader regions of your genome depending on what condition is suspected.
5. Pharmacogenomic Testing
Ever wondered why some medications work better for you than others? Pharmacogenomic tests show how your genes affect your response to medications.
This helps doctors prescribe the most effective drugs and dosages while helping you avoid adverse reactions. It directly impacts treatment safety and effectiveness across multiple medical specialties, from psychiatry to cardiology.
For example, this kind of test might show that you metabolize a certain medication slowly, so a lower dose would work better to avoid side effects.
By identifying genetic variants that influence how you process and respond to drugs, these tests help personalize your medication plan.
6. Prenatal & Newborn Screening
Prenatal tests check for genetic abnormalities during pregnancy, while newborn screening is done on infants soon after birth to detect rare genetic disorders early. About 1 in 300 newborns has a genetic condition that routine screening can detect, allowing prompt treatment to prevent serious problems.
Prenatal options include non-invasive screenings like cell-free DNA tests and more definitive but invasive procedures such as amniocentesis. Newborn screening programs vary by state but typically test for metabolic, endocrine, and blood disorders that benefit from early treatment.
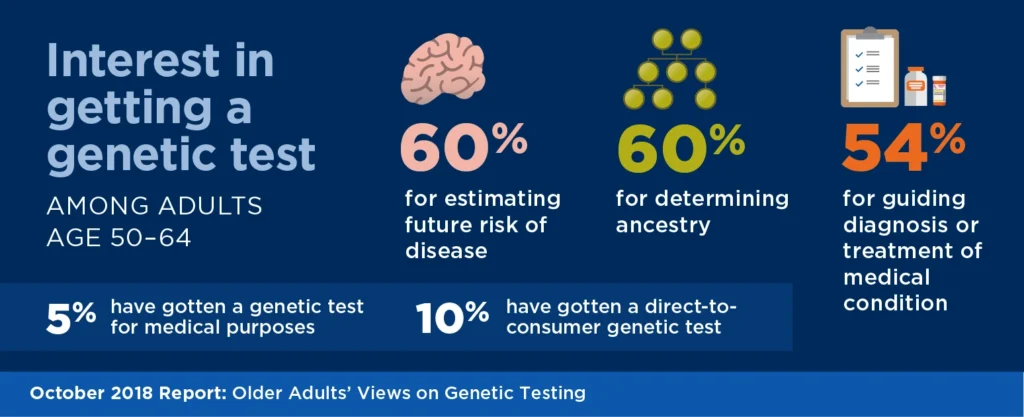
7. Direct-to-Consumer Testing (DTC)
You’ve probably seen ads for these tests. They’re commercially available and provide information about ancestry, traits, and some health risks without requiring a doctor’s involvement.
However, they typically offer less comprehensive health insights than clinical tests. While convenient and accessible, the interpretation often lacks the context that medical professionals provide. Many people use these tests as starting points for deeper exploration with healthcare providers.
The Pros of Genetic Testing
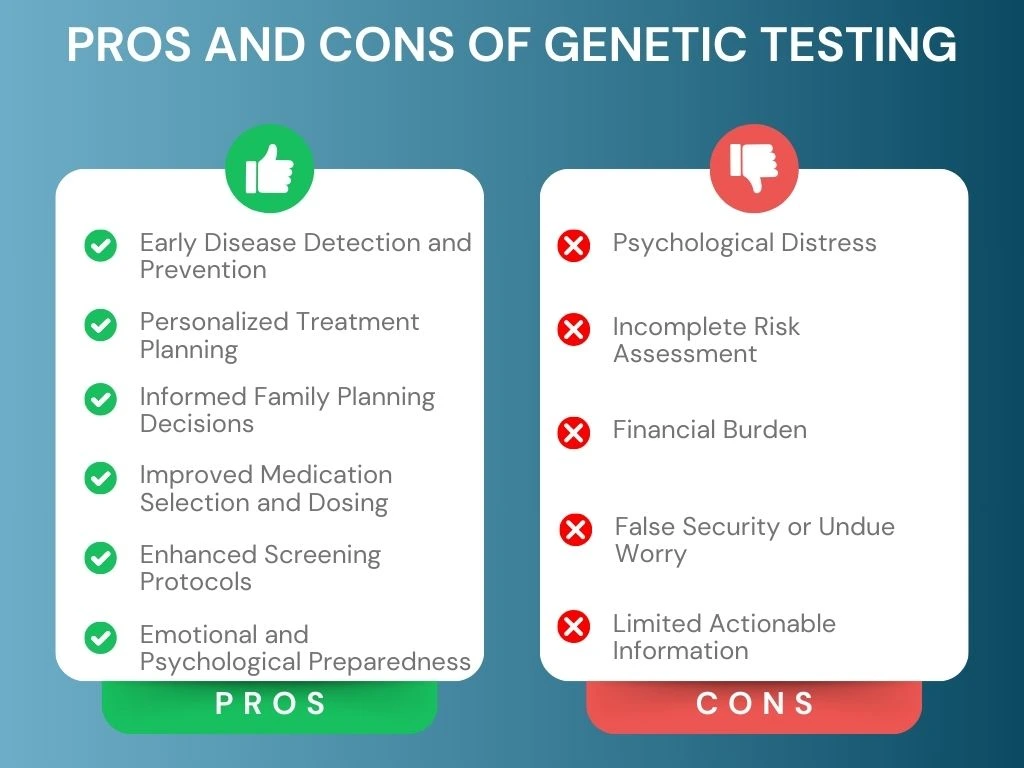
What are the potential benefits of genetic testing? Let’s explore the advantages that might make it worthwhile for you.
1. Early Disease Detection and Prevention
Genetic testing helps identify disease risks before symptoms develop. This early detection allows for preventive measures, enhanced screening, and lifestyle changes that may delay or prevent disease onset.
For example, if you know you have a genetic risk for a certain condition, you can start regular screenings or preventive measures sooner, which could be lifesaving.
2. Personalized Treatment Planning
Results from genetic tests help healthcare providers develop personalized medical care tailored specifically to your genetic profile.
This ensures more effective treatment strategies and reduces the trial-and-error approach to medication. For instance, a genetic test might identify a particular mutation in a tumor, pointing doctors to a targeted therapy rather than general guidelines that might not work as well for you.
3. Informed Family Planning Decisions
Planning to have children? With carrier testing, couples can find out if they carry any inherited conditions that they might pass on, and then consider options like special prenatal monitoring, IVF with genetic screening, or simply preparing for a child with that condition.
4. Improved Medication Selection and Dosing
Pharmacogenomic testing identifies how your genes influence your response to medications. This prevents adverse drug reactions and ensures optimal treatment effectiveness.
Instead of the “one-size-fits-all” approach, your doctor can match medications to your genetic profile. This can save you from unnecessary side effects and ineffective treatments.
5. Enhanced Screening Protocols
Knowing your genetic risk factors allows for customized screening schedules. If you’re at high risk, you’ll receive more frequent or specialized screenings.
For example, women with BRCA mutations might begin mammograms earlier and get additional imaging like MRIs. These tailored protocols significantly improve survival rates through earlier intervention. It’s a more precise approach to preventive health which is based on your individual risk profile.
6. Emotional and Psychological Preparedness
For some people, having clear information brings peace of mind. Even if the news isn’t ideal, knowing your genetic risks ahead of time allows you to prepare emotionally and make informed plans. And if the results are reassuring, you can shed worries about a condition you thought you might be at risk for.
The Cons of Genetic Testing
While there are clear benefits, genetic testing isn’t without drawbacks. Let’s examine the potential disadvantages of genetic testing.
1. Psychological Distress
Learning about genetic predispositions to serious conditions can trigger anxiety, depression, or fear. This is especially true when preventive or treatment options are limited.
The psychological burden of knowing your risk factors can be significant. How would you handle information about a disease risk you can’t control? This is an important question to consider before testing.
2. Incomplete Risk Assessment
Genetic tests often can’t predict disease severity, age of onset, or whether a condition will develop at all.
Many diseases result from complex interactions between multiple genes and environmental factors. This limits how accurately tests can predict your future health. It’s like having part of a map – helpful, but not the complete picture.
3. Financial Burden
Let’s be honest – genetic testing can be expensive. Costs range from hundreds to thousands of dollars, and insurance coverage varies widely.
This creates potential financial barriers for many people. The expense extends beyond the initial test to include genetic counseling, follow-up testing, and potentially increased surveillance based on results. For families needing multiple tests, these costs add up quickly.
In addition, not everyone has easy access to genetic specialists or counselors, especially in rural or underserved areas.
4. False Security or Undue Worry
Negative results might create a false sense of security, while positive results can cause excessive worry about conditions that may never develop.
A negative genetic test doesn’t eliminate all risks, as many conditions have multiple causes not captured by current testing. On the flip side, learning about genetic risks sometimes leads to anxiety disproportionate to the actual medical implications. This represents one of the key disadvantages of genetic testing which requires careful management.
5. Limited Actionable Information
For many identified genetic variants, clear medical interventions don’t exist. This limitation can leave you with knowledge of risk factors but no concrete steps to address them.
What’s the value of knowing if you can’t do anything about it? This question troubles many people considering genetic testing and represents a significant drawback in the overall pros and cons of genetic testing debate.
Major Challenges with Genetic Testing
Beyond the basic genetic testing pros and cons, there are some complex challenges associated with it. Let’s discuss these important considerations.
1. Responsibility of Sharing Genetic Information
What would you do if you discovered genetic risk factors that might affect your family members? This creates an ethical dilemma.
While sharing could benefit your relatives’ health management, it also raises privacy concerns and potential psychological impacts. The question becomes especially complex when relatives haven’t expressed interest in knowing their genetic risks or when family relationships are strained.
Genetic counseling helps navigate these decisions, balancing personal privacy with potential health benefits for relatives. Counselors can help you develop strategies for sharing information sensitively with family members.
At the end of the day, decisions about sharing genetic information reflect personal values, family dynamics, and the specific medical implications of the genetic variants identified.
2. Genetic Discrimination and Misuse of Data
Despite legal protections like the Genetic Information Nondiscrimination Act (GINA), concerns persist about how test results might be used against individuals.
Would your genetic information affect your life insurance, disability insurance, or employment opportunities? These fears cause some people to avoid potentially beneficial testing. Data security presents another challenge, as genetic information in databases could be vulnerable to breaches.
3. Post-Testing Care Coordination and Follow-Up
Care doesn’t end after receiving your test results. You need structured follow-up to ensure you fully understand your findings and next steps.
Ongoing care coordination between physicians and specialists is crucial to provide tailored recommendations. The benefits of electronic health records become evident here, as they allow all your healthcare providers to access your genetic information and integrate it with your complete medical history. Without proper care continuity, the value of genetic testing diminishes significantly.
4. Ethical Concerns in Reproductive and Prenatal Testing
Genetic testing in pregnancy and in vitro fertilization raises profound ethical questions. What decisions would you make with this information?
The ability to screen for genetic conditions before birth creates difficult decisions for prospective parents. Concerns about “designer babies” further complicate these discussions, raising moral questions about the appropriate limits of genetic testing in reproductive contexts.
Integrating Genetic Testing into Personalized Concierge Care
How can you get the most value from genetic testing? Let’s explore how it works best when integrated into comprehensive, personalized healthcare.
Immediate Physician Access for Genetic Consultations
Having quick access to a doctor when questions arise about your genetic test results makes a big difference. Unlike traditional healthcare, where results may be confusing or unexplained, direct access ensures you receive clear guidance without delays.
Concierge medical services provide this continuous access, allowing for timely discussions about complex genetic information. This immediate physician availability represents one of the key benefits of concierge medicine when dealing with genetic information. It addresses one of the major limitations of standalone testing – the gap between getting results and understanding what they mean for you.
The value becomes especially clear when new research emerges about previously identified genetic variants. As science evolves, so might the implications of your genetic findings. In a concierge model, you can quickly consult with your physician about how these developments affect your health management.
Proactive Health Management with Genetic Insights
Your genetic test results aren’t static information – they require interpretation and action. Physicians use this data to adjust health screenings, recommend preventive measures, and refine treatment plans based on your genetic risk factors.
In concierge family medicine, doctors integrate genetic insights with other health data, including biometric screening results and health risk assessment findings. This comprehensive approach enables truly personalized health strategies.
The benefits of telemedicine enhance this process by allowing for convenient follow-up discussions about your genetic findings. Similarly, telehealth in primary care provides greater access to genetic specialists regardless of your location, ensuring you receive expert guidance when needed.
Implementation often involves nuanced decisions about preventive interventions. For example, if you have genetic variants associated with increased heart disease risk, you might receive customized recommendations for exercise, nutrition, and medication – all specifically tailored to address your particular genetic vulnerabilities.
This level of precision represents the practical application of genetic knowledge – translating complex information into concrete lifestyle and medical interventions. The “what are the pros and cons of genetic testing” question finds its most meaningful answer in this translation from information to action.
Long-Term Support and Preventive Care Adjustments
Genetic testing is just the starting point. As new research emerges and your health conditions evolve, ongoing physician oversight ensures that care plans remain relevant and proactive.
Membership medicine provides the continuity needed to translate genetic insights into lasting health benefits. The emphasis on preventive health within concierge care models aligns perfectly with the predictive nature of genetic testing.
This approach becomes particularly valuable as you age and your risk profile changes. Genetic risk factors often interact with age-related changes, requiring periodic reassessment of preventive strategies. The continuous physician relationship in concierge models enables this evolving approach to genetic risk management.
Additionally, as family health histories expand over time with new diagnoses among relatives, the interpretation of your existing genetic information may shift. A doctor familiar with both your genetic profile and your evolving family history can integrate these insights more effectively than disconnected care systems.
Conclusion
Overall, genetic testing plays an increasingly valuable role in modern healthcare. It goes beyond identifying risks to enabling proactive, personalized health management when combined with good medical oversight.
The value of genetic information depends significantly on the healthcare context in which it’s delivered and applied. By combining genetic testing with consistent physician guidance, you can make more informed health decisions and implement tailored prevention strategies.
At the end of the day, weighing the pros and cons of genetic testing is a personal decision that depends on your specific health concerns, family history, and preferences. As testing becomes more mainstream – with 40% of Americans having had at least one test – the focus shifts to ensuring this information translates into meaningful health improvements.
Are you considering genetic testing? Exploring healthcare solutions tailored to your needs is essential. WorldClinic offers comprehensive concierge medical services that integrate genetic insights into personalized health planning, providing the support and expertise needed to transform genetic information into meaningful health actions. Contact us today to learn how we can help you.
Experience Personalized Healthcare Anywhere, Anytime
Discover how WorldClinic’s Concierge Telemedicine Services put world-class medical expertise at your fingertips. From 24/7 access to tailored medical solutions, our memberships ensure peace of mind and proactive care for you and your family.
FAQs About Genetic Testing
1. Who should consider genetic testing?
You should consider genetic testing if you have a family history of genetic disorders, are planning a pregnancy, have unexplained symptoms that might have a genetic cause, or want to understand your risk for certain conditions. It’s especially valuable if you have close relatives who developed diseases at young ages or if you belong to an ethnic group with higher risks for specific genetic conditions.
2. How does genetic testing impact treatment plans and medical decisions?
Genetic testing directly influences treatment by helping doctors select the most effective medications based on how your body will process them, determine appropriate screening schedules, and implement preventive measures before symptoms appear.
3. How long does it take to receive genetic test results?
The timeline for genetic test results varies by test type. Simple tests might return results in 1-2 weeks, while comprehensive genetic panels can take 4-8 weeks. Urgent tests, like those done during pregnancy, may be expedited. The complexity of analysis, lab backlogs, and insurance approval processes all affect timing.
4. How often should I update or retake a genetic test?
Most genetic tests don’t need to be repeated since your DNA doesn’t change. However, you should consider updates when: new family health information emerges, you’re planning a pregnancy, new testing technology becomes available that examines more genes, or research advances change the interpretation of your previous results.
5. How does genetic testing fit into a personalized healthcare plan?
Genetic testing serves as a foundation for truly personalized healthcare by providing insights that guide prevention strategies, screening schedules, medication choices, and lifestyle recommendations. In a comprehensive healthcare plan, genetic information works alongside other health data like family history, biometric screening results, and ongoing monitoring.


