The current U.S. healthcare system operates within a financial framework that is, in many ways, at odds with the goal of delivering individualized, high-quality care. Rising costs have gradually placed a strain on patients who find themselves juggling medical expenses and on providers who are forced to make tough decisions between quality and affordability. It’s a reality that’s neither new nor surprising, yet it continues to push both patients and providers toward a critical juncture.
In response, utilization management has emerged as a practical tool, not for limiting care but for reshaping how it’s delivered. By emphasizing efficiency and medical necessity, it seeks to align treatments with genuine patient needs while keeping financial waste in check. This system isn’t about withholding; it’s about refining how we manage resources—ensuring they are directed where they provide the most benefit, both clinically and financially. Throughout this blog, walk through the core concepts of utilization management in healthcare. We’ll look at the utilization review process, examine the benefits and challenges, and take a closer look at the role concierge medicine plays in ensuring that each patient receives the care they need without compromising on quality or value.
What is Utilization Management in Healthcare?
Utilization management serves as a disciplined framework within healthcare, one that ensures medical care aligns with true necessity while maintaining a sharp focus on cost control. It’s a system employed by both healthcare providers and insurers, used to evaluate treatments, procedures, and services through a meticulous lens—measuring each against criteria of efficiency and clinical relevance.
This meticulous process seeks to guide healthcare away from excess and waste without compromising quality. By adhering to evidence-based guidelines, it filters out unnecessary tests and extended hospital stays, avoiding resource depletion. More simply put, the aim is to ensure the patient gets exactly what they need while not losing sight of what’s medically sound and financially sustainable.
What Is a Utilization Review?
The utilization review process operates as the fine-tuned mechanism within the broader structure of utilization management that thoroughly assesses the necessity of medical interventions at three distinct stages:
Stage 1: The Prospective Review
A prospective review primarily acts as the first “filter” in analyzing the validity of proposed treatments and takes place before any treatment begins.
This phase is often used to authorize procedures or treatments that may carry significant costs or risks. Whether it’s a procedure or an extended treatment plan, this review aims to curtail superfluous interventions, safeguarding both the patient and the system from avoidable costs and ineffective care.
Stage 2: The Concurrent Review
During active treatment, the concurrent review engages in a more dynamic process—tracking the real-time progress of a patient’s care. It’s a mechanism that ensures the prescribed treatment remains relevant and necessary as the clinical situation evolves. Any deviation from the anticipated course is caught early, allowing for adjustments that protect the integrity of the treatment plan and preventing care from becoming an unchecked process that outpaces its purpose.
Stage 3: The Retrospective Review
Retrospective reviews look backward after care has concluded. It examines the entire episode of care with the benefit of hindsight, revealing areas where inefficiencies may have slipped through and where improvements can be made in the future. It also assesses whether the care delivered was both appropriate and cost-efficient, feeding this analysis back into the system to refine future decisions.
Benefits of Utilization Management in Healthcare

1. Cost Reduction
As we’ve seen, healthcare utilization management takes a deliberate approach to curb costs. Unnecessary procedures are intercepted before they materialize, redundant tests are filtered out, and excessive treatments are trimmed. Every service must be justified to ensure that what is spent aligns with what is needed, leading to measurable savings across the system. For instance, one study on high-need, high-cost Medicaid patients showed that using management practices, including case management and care coordination, led to a 37% reduction in total medical costs and a 59% decrease in inpatient utilization.
2. Improved Patient Outcomes
When care aligns with established clinical evidence, patient outcomes improve as a matter of course. Utilization management facilitates this alignment. This structured approach to treatment accelerates recovery, reduces the risk of complications, and keeps patients from lingering in hospitals longer than necessary. Fewer unnecessary treatments mean fewer adverse events, fewer complications, and lower readmission rates. In fact, a systematic review of hospital utilization management strategies found that techniques, such as pre-admission authorizations and concurrent reviews, led to a reduction in hospital admissions by approximately 12%.
3. Efficient Resource Allocation
In an environment like healthcare where demand frequently outstrips capacity, the ability to allocate resources efficiently is critical. Utilization management acts as a mechanism for identifying and prioritizing patient needs, ensuring that the right resources—whether it’s staff time, specialized equipment, or clinical expertise—are directed where they can have the greatest impact. This targeted approach not only reduces waste but also helps mitigate patient wait times and overcrowding, leading to more streamlined operations. For example, a report from the Institute for Healthcare Improvement (IHI) has shown that hospitals that implement efficient patient flow strategies can significantly reduce unnecessary admissions and streamline the prioritization of critical cases, leading to enhanced resource management.
4. Enhanced Care Coordination
Fragmented care often results in disjointed treatment plans, poor communication between providers, and ultimately, suboptimal patient outcomes. Effective utilization management actively fosters better care coordination by aligning every step of the treatment process with a carefully evaluated plan.
This level of oversight ensures that care providers—whether they’re specialists, primary care physicians, or hospital staff—are all working toward the same objectives. Naturally, better healthcare coordination reduces medical errors, improves patient adherence to treatment plans, and minimizes redundant tests or conflicting treatments. By guiding transitions between providers and ensuring that care remains cohesive, it promotes smoother, more effective care pathways.
5. Improved Compliance with Standards
Processes, such as prior authorization and concurrent reviews, ensure that healthcare providers follow evidence-based practices. By evaluating treatments through this lens, utilization management helps healthcare providers comply with state and federal regulations, medical necessity criteria, and their duty of care to patients. This alignment not only promotes the delivery of appropriate care but also reduces legal risks and financial liabilities for both providers and payers.
Organizations accredited by bodies like URAC and NCQA are required to adhere to stringent standards, which include the use of objective, evidence-based criteria for decision-making. This helps ensure that medical services are provided in accordance with regulatory guidelines, reducing the likelihood of non-compliance and legal exposure.
6. Patient Satisfaction
Patients today demand transparency and efficiency in their care. Utilization management directly contributes to this by ensuring that treatments are clearly necessary and that patients are not subjected to tests or procedures of dubious value. As a result, patients can feel more confident in the care they receive, knowing that it is driven by necessity rather than excess. This not only reduces anxiety but fosters a greater sense of trust in the healthcare system. Additionally, patients who experience shorter hospital stays, faster recoveries, and fewer complications are, unsurprisingly, more satisfied with their overall care experience.
Challenges of Utilization Management in Healthcare
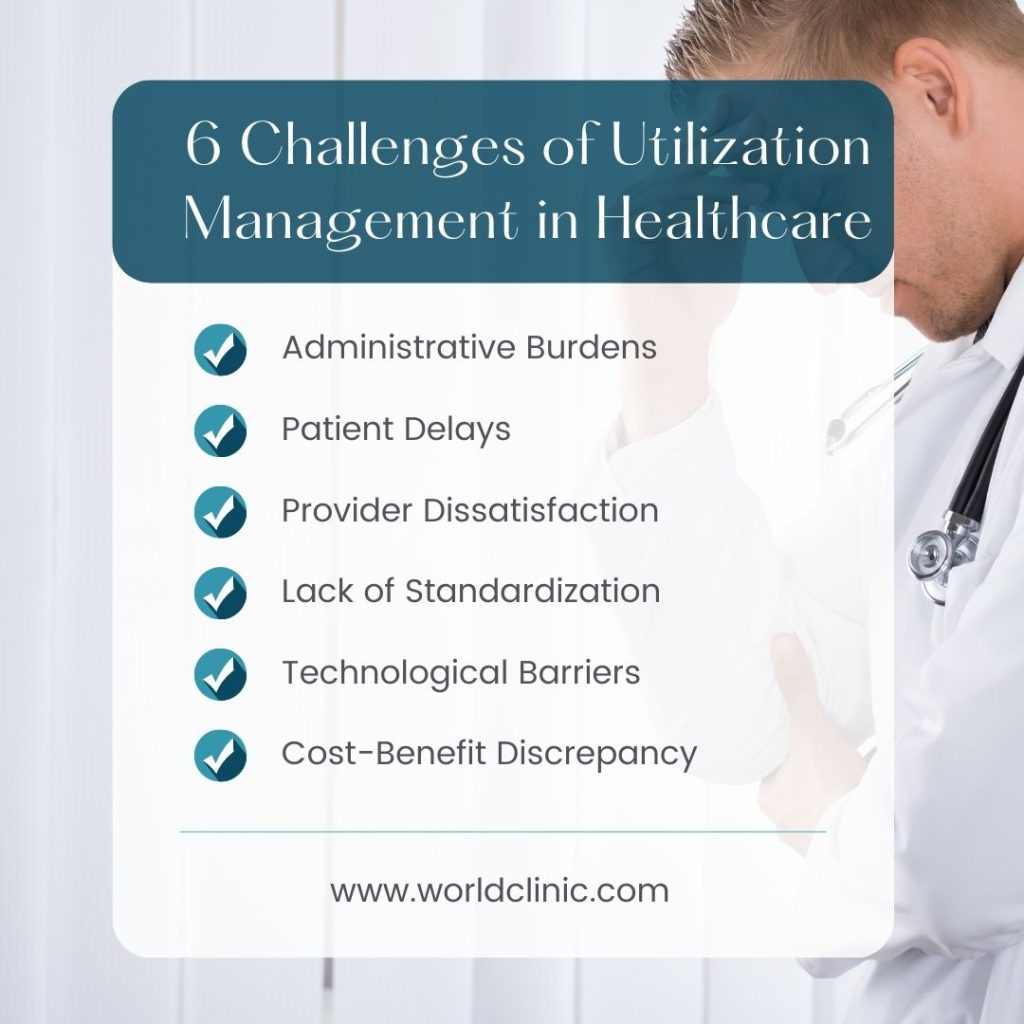
For all the clear benefits, healthcare organizations face several challenges in its implementation.
1. Administrative Burdens
One of the most immediate challenges is the increased administrative workload. Utilization management demands a higher level of documentation and detailed oversight, which translates to more paperwork and system inputs for healthcare providers. This burden can slow down the entire care process, forcing physicians and staff to divert time and energy away from direct patient care. The layers of approvals and compliance checks can feel like an impediment, leading to a sense that the process is bureaucratically heavy-handed rather than clinically beneficial.
2. Patient Delays
The very processes that aim to ensure efficiency can sometimes inadvertently delay care. Prior authorizations, where providers must obtain approval before moving forward with treatments or procedures, are notorious for causing delays. These delays, while intended to ensure that care aligns with medical necessity, can inadvertently push back treatment start times, potentially impacting patient outcomes.
3. Provider Dissatisfaction
Many physicians express dissatisfaction with utilization management processes, often feeling that it undermines their clinical judgment. The need to secure approvals for treatments they deem necessary introduces delays and, at times, frustrates the patient-provider relationship. Physicians may feel that the time spent on administrative tasks detracts from their ability to focus on patient care, leading to a sense of dissatisfaction that can ripple through the healthcare experience. This strain has the potential to erode the trust and rapport between doctor and patient, which is critical for successful care delivery.
3. Lack of Standardization
One of the more significant challenges lies in the lack of uniformity across processes. Different healthcare organizations and insurers apply varying criteria for authorizations and reviews, which creates inefficiencies. Physicians and healthcare staff often find themselves struggling with different systems and guidelines, leading to confusion and delays. The absence of a standardized approach complicates efforts to streamline the process, as providers are forced to navigate a patchwork of requirements that differ based on the payer or organization.
5. Technological Barriers
Effective utilization management relies heavily on up-to-date technology and infrastructure, yet not all healthcare providers have access to the tools required for efficient implementation. Outdated systems or a lack of integration between different departments or insurers can impede the smooth execution of processes. Electronic health records (EHRs) and other digital platforms need to be able to support utilization management without adding extra steps for the provider. Understanding the benefits of electronic health records is essential to recognizing their potential to streamline processes and reduce errors. Without adequate technology, manual processes prevail, slowing down approvals and increasing the risk of errors. This lack of technological readiness can make implementation more cumbersome than beneficial.
6. Cost-Benefit Discrepancy
While utilization management seeks to reduce unnecessary costs, the systems themselves are not without expense. Developing and maintaining a robust system requires financial and human resources, and for some organizations, the cost of running the program may outweigh the savings. This cost-benefit discrepancy can create tension, particularly for smaller healthcare providers or organizations operating on tight margins, as they try to balance the immediate costs with the potential long-term financial savings.
Utilization Management in Concierge Medicine: A Personalized Approach
Despite the challenges, solutions exist. WorldClinic integrates utilization management principles into our care model to ensure patient needs are met efficiently and effectively. We do this through:
Proactive Care Coordination
We employ an anticipatory model of care coordination. Rather than reacting to fragmented episodes of treatment, we ensure that all providers are in sync from the outset. This means continuous oversight across every aspect of the patient’s health, eliminating the inefficiencies that come with delayed communication. Patients move through their care plans without encountering the stumbling blocks often seen in traditional systems, where lapses in coordination create unnecessary delays.
Direct Access to Healthcare Providers
Immediate access to care reframes how decisions are made. Rather than waiting through endless layers of approval, WorldClinic gives patients the ability to consult their physician when they need it—whether for routine concerns, urgent matters, or doctor referrals. This direct connection allows real-time adjustments in care, avoiding the common delays that hamper treatment progress. It’s tailored access that ensures patients get answers, decisions, and treatment without unnecessary waits.
Customized Health Plans
Every patient brings a unique health narrative, and our model is dedicated to supporting that. Every health plan that is created for our members is crafted from a deep understanding of the patient’s history, preferences, and unique health goals. This customization is essential as it allows for a deeper alignment between the patient’s needs and the care they receive, ensuring that treatment not only addresses immediate concerns but adapts as circumstances evolve.
Conclusion
As we can see, utilization management provides a structured way to deliver care that balances necessity with efficiency, but its true impact lies in how it’s applied. By offering immediate access to providers, seamless coordination, and carefully crafted health plans, we at WorldClinic transform the principles of utilization management into real-world solutions that work for both patients and healthcare systems. If you’re looking for a URAC-accredited healthcare partner who understands the importance of timely, tailored care, contact us today. Let us bring the same precision and personalization to your health that has made us a trusted name in concierge medical services.
Utilization Management in Healthcare FAQs
How does utilization management differ from traditional medical management?
Utilization management focuses on evaluating the necessity, efficiency, and appropriateness of care before, during, and after treatment. Traditional medical management tends to be less structured in assessing whether specific treatments or services are truly necessary.
What types of healthcare services are most commonly subject to utilization management?
High-cost treatments, surgeries, hospital stays, diagnostic tests, and specialty care services often undergo utilization management to ensure medical necessity and cost-effectiveness.
What are utilization management rules and guidelines?
These are evidence-based protocols that guide decisions on the appropriateness of care. They help ensure that treatments align with medical standards and regulatory requirements while minimizing waste.
What role does technology play in enhancing utilization management?
Technology streamlines the process by enabling real-time data analysis, automating approvals, and improving communication between healthcare providers, all of which contribute to faster, more efficient decision-making.
What are three important functions of utilization management?
Utilization management serves to prevent unnecessary treatments, ensure that care aligns with clinical guidelines, and optimize the allocation of healthcare resources.
What are the legal implications of utilization management for healthcare providers?
Utilization management imposes a responsibility on providers to ensure that care meets established guidelines. Failure to adhere to these standards can expose providers to legal risks, including claims of improper care or regulatory penalties for non-compliance.


